SUDHAMSHI REDDY
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis
45 year old male came to OPD with chief complaints of:
1. Constipation since 3 days
2. Pain in abdomen since 2days
3. Vomitings since 2 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 days ago then he developed pain in the abdomen- in epigastric region.
It was sudden in onset, gradually progressive.
Pain more after eating food and on lying in supine position.
Pain relieved on sitting , on bending forward.
-H/O 3 episodes of Vomiting yesterday after eating food, food as content, non bilious, non projectile, not blood tinged.
-Constipation since 3 days
No H/O fever, cough, cold, shortness of breath, loose stools, giddiness.
Last binge of alcohol consumption 2days ago.
PAST HISTORY:
H/O similar complaints 2 years ago- diagnosed as Acute pancreatitis, treated at KIMS Narketpally
Not a K/C/O DM, HTN, TB, Asthma, Epilepsy,CVA,CAD
PERSONAL HISTORY:
He is a carpenter by occupation
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel and bladder regular
Consumes 2 quarters of alcohol/day since 20 years
FAMILY HISTORY
No significant family history
GENERAL EXAMINATION
Patient is conscious , coherent and cooperative. Well oriented to time place and person.
No signs of pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy, edema
VITALS:
Pulse - 76 bpm
BP - 110/80 mm Hg
RR - 18 cpm
Temp- 97.8F
SpO2- 98% on room air
GRBS- 124mg%
SYSTEMIC EXAMINATION:
P/A-
INSPECTION:Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Percussion over abdomen- tympanic note heard.
Bowel sounds -sluggish

RS: BAE ,NVBS, no added sounds
CVS : S1 ,S2 heard no murmurs
CNS:
HIGHER MENTAL FUNCTIONS- INTACT
MEMORY- able to recognise his family members and recall recent events
SPEECH: normal
CRANIAL NERVE EXAMINATION- normal
REFLEXES-
RIGHT LEFT
BICEPS 2+ 2+
TRICEPS 2+ 2+
SUPINATOR 1+ 1+
KNEE 2+ 2+
ANKLE. 2+ 2+
SUPERFICIAL AND DEEP REFLEXES ARE PRESENT AND NORMAL
MUSCLE POWER-
RIGHT LEFT
UPPER LIMB
ELBOW 5/5 5/5
WRIST 5/5 5/5
HAND GRIP 5/5 5/5
LOWER LIMB
HIP 5/5 5/5
KNEE. 5/5 5/5
ANKLE 5/5 5/5
TONE- NORMAL IN UPPER AND LOWER LIMBS
NO INVOLUNTARY MOVEMENTS
SENSORY SYSTEM- ALL SENSATIONS ARE NORMAL
RANSONS CRITERIA
on admission
1. WBC >16,000/MICROLITRE-0
2.Age>55 yrs- 0
3. Glucose >200 mg/dl-0
4. AST>250 IU/L-0
5. LDH>350IU/K
BISAP SCORE
1. BUN>25-0
2. Impaired mental status-0
3. SIRS-1
4. Age>60-0
5. Pleural effusion- 0
SIRS
Two or more of the following criteria
1. Heart rate > 90
2. Temp > 100.4°F (38°C) or < 96.8°F (36°C)
3. Respiratory rate > 20 or PaCO2 < 32 mm Hg
4. WBC > 12,000/mm³ or < 4,000/mm³, or > 10% band forms
Dermatology opinion taken I/v/o itchy skin lesions over left foot since 10years, diagnosed as LICHEN SIMPLEX CHRONICUS, adviced
1. PROPYSALIC NF OINTMENT L/A OD x 1week
2. VENUSIA MAX LOTION L/A BD X 4weeks
8/4/23
Hb-16.3 gm/dl
TLC-14100 cells/cu.mm
PLT- 2.16 lakhs/cu.mm
RBC- 5.18 million/cu.mm
9/4/23
Hb- 15.6
TLC-11500
PLT-1.87
RBC- 4.94million/cu.mm
10/4/23
Hb- 16.7
TLC-10,300
PLT-1.98
RBC- 5.42
11/4/23
Hb- 16.0
TLC- 9500
PLT- 1.87
RBC- 5.10
CUE:
Albumin- +
Pus cells- 3-4
Epithelial cells- 2-3
8/4/23
Blood urea- 36mg/dl
Serum creatinine - 1.0mg/dl
11/4/23
Blood urea- 30mg/dl
Serum creatinine- 0.8mg/dl
LFT:
TB- 1.17mg/dl
DB- 0.26mg/dl
SGOT- 45IU/L
SGPT- 41IU/L
ALP- 166IU/L
TP- 6.9 gm/dl
Alb- 4.3 gm/dl
A/G- 1.67
8/4/23
Na-140
K-4.1
CL-102mmol/l
9/4/23
Na-139
K-3.5
CL-102
11/4/23
Na- 140
K-3.4
Cl-98
Serum amylase- 841
Serum lipase- 218
RBS-121mg/dl
Lipid profile
TC- 185
TG- 130
HDL- 52
LDL-108
VLDL-26
ECG-
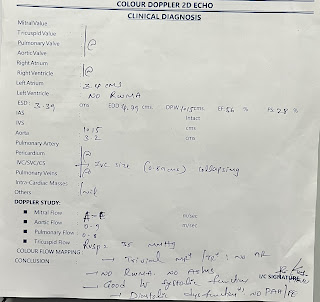
2D ECHO-
USG ABDOMEN-
CHEST X RAY
PROVISIONAL DIAGNOSIS:
RECURRENT ACUTE PANCREATITIS - INTERSTITIAL
ALCOHOL DEPENDENT SYNDROME
LICHEN SIMPLEX CHRONICUS
TREATMENT:
1.NBM TILL FURTHER ORDERS
2.IV FLUIDS 1Unit NS BOLUS @100ml/hr
2 units NS, RL, 1Unit DNS
3.INJ TRAMADOL 1amp in 100ml NS IV over 1hr/BD
4.INJ THIAMINE 1amp in 100ml NS IV/BD
5.INJ PAN 40mg IV/OD
6.INJ ZOFER 4mg IV/TID
SOAP NOTES:
9/4/23
S
Abdominal pain subsided
Flatus-not passed
No fever spikes
Stools not passed since 4 days
O
Pt is conscious , coherent , cooperative
BP-130/80mmHg
PR- 84bpm
Temp- 98.2F
RR-18 cpm
Input/output-3000/900ml
GRBS-96mg/dl
CVS- S1,S2 heard, no murmurs
RS- BAE (+), NVBS(+)
P/A-mild tenderness in epigastric region
Bowel sounds-5/minute
CNS: NAD
A
RECURRENT ACUTE PANCREATITIS INTERSTITIAL
P
1. NBM TULL FURTHER ORDERS
2. IV FLUIDS - 2 UNITS MS, 2 UNITS RL, 2 UNITS DNS @125 ML
3.INJ TRAMADOL 1amp in 100ml NS IV over 1hr/BD
4.INJ THIAMINE 1amp in 100ml NS IV/BD
5.INJ PAN 40mg IV/OD
6.INJ ZOFER 4mg IV/TID
7. SYP LACTULOSE15 ML PO/HS
10/4/23
S
Abdominal pain subsided
Fever spikes @ 9pm
Stools not passed since yesterday
O
Pt is conscious , coherent , cooperative
BP-120/80mmHg
PR- 92 bpm
Temp- 98.2F
RR-18 cpm
Input/output-3200/1400ml
GRBS-118mg/dl
CVS- S1,S2 heard, no murmurs
RS- BAE (+), NVBS(+)
P/A- Soft,no tenderness, no organomegally
Bowel sounds present
CNS: NAD
A
RECURRENT ACUTE PANCREATITIS- INTERSTITIAL
ALCOHOL DEPENDENCE SYNDROME
P
1. NBM TULL FURTHER ORDERS
2. IV FLUIDS - 2 UNITS MS, 3 UNITS RL, 2 UNITS DNS @125 ML
3.INJ TRAMADOL 1amp in 100ml NS IV/SOS
4.INJ THIAMINE 1amp in 100ml NS IV/BD
5.INJ ZOFER 4mg IV/SOS
6. SYP LACTULOSE15 ML PO/BD
11/4/23
S
No fever spikes
Stools not passed
Tolerating oral fluids
O
Pt is conscious , coherent , cooperative
BP-120/80mmHg
PR- 92 bpm
Temp- 98.2F
RR-18 cpm
Input/output-2700/1300ml
GRBS-92mg/dl
CVS- S1,S2 heard, no murmurs
RS- BAE (+), NVBS(+)
P/A- Soft,no tenderness, no organomegally
Bowel sounds present
CNS: NAD
A
RECURRENT ACUTE PANCREATITIS- INTERSTITIAL
ALCOHOL DEPENDENCE SYNDROME
LICHEN SIMPLEX CHRONICUS
P
1. Liquid diet-->soft diet
2. IV FLUIDS - 1 UNIT NS, 2 UNITS RL, 1 UNIT DNS @125 ML
3. INJ TRAMADOL 1amp in 100ml NS IV/SOS
4. INJ THIAMINE 1amp in 100ml NS IV/BD
5. INJ ZOFER 4mg IV/SOS
6. SYP LACTULOSE15 ML PO/BD
7. Tab LORAZEPAM 2mg PO/OD
8. Tab. BACLOFEN 20MG PO/OD
9. PROPYSALIC NF ointment L/A ODx1 week
10. VENOSIA MAX LOTION L/A BD x4 weeks
12/4/23
S
No complaints of nausea and vomiting
No fever spikes
Stools passed
O
Pt is conscious , coherent , cooperative
BP-130/80mmHg
PR- 88 bpm
Temp- 96.8F
RR-18 cpm
Input/output-2380/1050ml
GRBS-108mg/dl
CVS- S1,S2 heard, no murmurs
RS- BAE (+), NVBS(+)
P/A- Soft,no tenderness, no organomegally
Bowel sounds present
CNS: NAD
A
RECURRENT ACUTE PANCREATITIS- INTERSTITIAL
ALCOHOL DEPENDENCE SYNDROME
LICHEN SIMPLEX CHRONICUS
P
1. Plenty of oral fluids
2. soft diet -->normal diet
3. Tab THIAMINE 200 MG PO/BD
4. Tab ULTRACET 1/2 tab PO/SOS
5. SYP LACTULOSE 15 ML PO/HS
7. Tab LORAZEPAM 2mg PO/OD
8. Tab. BACLOFEN 20MG PO/OD
9. PROPYSALIC NF ointment L/A ODx1 week
10. VENOSIA MAX LOTION L/A BD x4 weeks









Comments
Post a Comment