40 YEAR OLD MALE WITH CHEST PAIN UNDER EVALUATION
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
COMPLAINTS AND DURATION:
Chest pain and pain in interscapular area since 5 years.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently alright 10 years ago then he started having on and off chest pain ( once in 2-3 months).
Since 5 years it has aggravated, episodes of pain once in every 7-8 days.
Pain radiates to back.
Nature of pain- heaviness/ tightness of chest and stiffness of back.-
-H/O mild shortness of breath if the episode of chest pain is severe
Pain triggers on eating sweets, non veg food and drinking milk, even on not having food for long period of time.
Relieves on taking Tab Nexpro RD and SUCRAFIL syrup.
- Chest pain relieved on walking, belching and passing flatus, passing stools.
-Regurgitation of food present
-C/O incomplete evacuation of stools next day after the episode of chest pain. No change in colour or consistency.
PAST HISTORY:
K/C/O Hypertension since 7 years on Tab Amlodipine+Metoprolol PO/OD
K/C/O Hemorrrhoids 3 years ago, relieved 1 year ago on taking homeopathic medication.
Not a k/c/o DM, Asthma, TB, Epilepsy, CAD, CVA.
PERSONAL HISTORY:
Normal appetite, takes mixed diet, sleep adequate with regular bowel and bladder habits.
No known addictions, allergies.
GENERAL EXAMINATION:
PT IS C/C/C
PALLOR: PRESENT
NO ICTERUS, CYANOSIS, CLUBBING, PEDAL EDEMA, LYMPHADENOPATHY.
VITALS ON ADMISSION:
PR-72 BPM
BP- 140/100MM HG
RR- 18 CPM
SPO2- 98%AT RA
SYSTEMIC EXAMINATION:
1) PER ABDOMEN:
2)RESPIRATORY SYSTEM:
BAE+
NORMAL VESICULAR BREATH SOUNDS HEARD
NO ADVENTITIOUS SOUNDS HEARD.
3) CVS:
S1,S2 +
NO THRILLS, NO MURMURS.
4) CNS:
PATIENT WAS C/C/C.
HIGHER MENTAL FUNCTIONS- INTACT
GCS - E4V5M6
B/L PUPILS - NORMAL SIZE AND REACTIVE TO LIGHT
NO SIGNS OF MENINGEAL IRRITATION.
CRANIAL NERVES- INTACT.
SENSORY SYSTEM-NORMAL.
MOTOR SYSTEM:
TONE- NORMAL
POWER- 5/5 IN ALL LIMBS
REFLEXES:
B/L REFLEXES: BICEPS - 2+, TRICEPS-2+, SUPINATOR + , KNEE - 2+, ANKLE - 2+
COURSE IN THE HOSPITAL:
PATIENT CAME WITH COMPLAINTS OF CHEST PAIN AND PAIN IN INTERSCAPULAR AREA SINCE 5 YEARS. THOROUGH CLINICAL EXAMINATION AND INVESTIGATIONS WERE DONE. ECG REVEALED NORMAL SINUS RHYTHM, CHEST X RAY REVEALED NO ABNORMALITY, ON USG ABDOMEN NO SONOLOGICAL ABNORMALITY WAS DETECTED.
PATIENT IS A KNOWN HYPERTENSIVE, ON MEDICATION Tab STARPRESS AM XL-50 PO/OD
REFERRED TO DERMATOLOGY (16/2/23) I/V/O SCALY LESIONS OVER SCALP SINCE 5-6 YEARS.
Advised: HALOX-S LOTION L/A x 2 WEEKS
( every alternate day)
REFERRED TO GASTROENTEROLOGY (17/2/23) I/V/O ?ACUTE GASTRITIS, UPPER GI ENDOSCOPY WAS DONE IT SHOWED MUTIPLE ACUTE GASTRO DUODENAL ULCERS.
PATIENT IS BEING DISCHARGED IN A HEMODYNAMICALLY STABLE CONDITION.
INVESTIGATIONS:
HEMOGRAM:
Hb- 13.6gm/dl
TLC-8000 cells/cu.mm
N/L/E/M- 60/33/1/6
PLT- 2.30 lakhs/cu.mm
RFT
UREA-27mg/dl
CREATININE-1mg/dl
URIC ACID -6.4
Ca- 9.4 mg/dl
Phos-2.2mg/dl
Na- 139 mEq/l
K- 4.4 mEq/l
Cl-103 mEq/l
FBS- 87mg/dl
PLBS- 105mg/dl
LIPID PROFILE:
Total cholesterol- 218mg/dl
TG- 222mg/dl
HDL- 42mg/dl
LDL-96mg/dl
VLDL- 44.4mg/dl
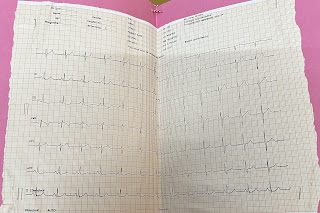
ECG:
CXR:
USG ABDOMEN- NO SONOLOGICAL ABNORMALITY DETECTED.
UPPER GI ENDOSCOPY:
IMPRESSION-MULTIPLE GASTRO DUODENAL ULCERS.
DIAGNOSIS:
GASTRODUODENAL ULCER
TREATMENT:
1. Tab STARPRESS AM XL-50 PO/OD
( METOPROLOL 50mg+ AMLODIPINE 5mg)
8AM—-x—-x
2. Tab MVT PO/OD
x—-2PM—-x
ADVICE AT DISCHARGE:






Comments
Post a Comment