SUDHAMSHI REDDY M
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
63 year old male agricultural worker by occupation came with chief complaints of
- B/L knee joint pain since 1 year
- Back pain since 1 year
- Neck pain since 4-6months
HISTORY OF PRESENTING ILLNESS:
Patient was apparently normal 1 year back he then had
- Pain in both the knee joints- insidious in onset, gradually
progressive. Early morning stiffness present.
Pain aggravated on walking long distances, relieved on
resting.
- C/O lower back pain since 1 year, insidious in onset,
gradual in progression, aggravated on working by
bending forward or lifting weights.
Non radiating
Tingling sensation present.
- C/O neck pain since 4-6 months, radiating towards both
shoulders.
No tingling sensation.
-C/O dull dragging type of pain in the centre of chest
non radiating , aggravated on exertion and relieved by
rest .
Not associated with SOB, palpitations, giddiness,
sweating
-C/O pain and tingling sensation in both feet.
-H/O an attack of giddiness 3 days back associated with
loss of consciousness , regained consciousness within
1minute and was normal without any confusion.
-No h/o fever, pain abdomen, burning micturition .
PAST HISTORY:
No similar complaints in the past
Not a k/c/o DM,HTN ,TB ,Asthma ,CVA, CAD ,Epilepsy, Thyroid disorders.
Surgical history-
Operated for Right eye SIMC 10 yrs back
PERSONAL HISTORY:
Diet mixed
Appetite normal
Sleep normal
Bowel and Bladder Regular
Occasional alcoholic drinks once in 10-15 days since 10 years.
Non smoker.
GENERAL EXAMINATION:
O/E
Patient is conscious coherent cooperative
No signs of pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy, edema.
VITALS:
Afebrile on touch
PR : 88bpm
RR : 18cpm
BP : 140/90 mm hg
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM:
INSPECTION:
Chest is bilaterally symmetrical
Trachea – midline in position.
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally with respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper/mid/lower interscapular were all RESONANT.
AUSCULTATION:
Normal vesicular breath sounds heard
No adventitious sounds heard.
CARDIOVASCULAR SYSTEM:
INSPECTION:
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse and pulsations cannot be appreciated
PALPATION:
Apical impulse is felt on the left 5th intercoastal space 2cm away from the midline.
No parasternal heave, thrills felt.
PERCUSSION:
Right and left heart borders percussed.
AUSCULTATION:
S1 and S2 heard , no added thrills and murmurs heard.
PER ABDOMEN:
INSPECTION:
Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Percussion over abdomen- tympanic note heard.
AUSCULTATION:
Bowel sounds are heard.
CENTRAL NERVOUS SYSTEM EXAMINATION:
Higher mental functions - intact
Straight Leg raising test:
Patient complains of pain at 60 degrees in left lower limb and at 45 degrees in right lower limb.
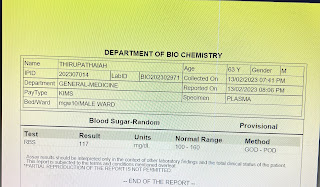
INVESTIGATIONS:
CXR
X-RAY C SPINE:
Lateral view-
AP view-
X-RAY B/L KNEE JOINT:
Lateral view-
AP view-
X-RAY LS SPINE
AP view-
LATERAL view-
2D ECHO-
USG ABDOMEN-
PROVISIONAL DIAGNOSIS:
Back pain under evaluation
? B/L knee osteoarthritis
Cervical spondylosis.
TREATMENT:
1. Tab ULTRACET PO/BD
2. Tab PAN 40mg PO/OD
REFERRAL NOTES:
Orthopaedic referral
























Comments
Post a Comment