SUDHAMSHI REDDY M
MBBS 9th semester
Roll no:80
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
42 year old male complaining of abdominal distension since 4 days, loss of appetite and not passing stools since 2 days.
Following is a brief about the case,
(History as per date of admission).
CHIEF COMPLAINTS:
A 42 year old male, butcher by occupation came to the casualty with complaints of:
• Lethargy since 1week.
• Abdominal distension since 4 days, loss of appetite and not passing stools since 2 days.
HISTORY OF PRESENT ILLNESS:
Patient is a butcher by occupation.
4 years ago he visited hospital because of abdominal pain, in the epigastric region, non radiating, is was not associated with any vomiting.
He was diagnosed with Diabetes mellitus then and was prescribed T.Gliclazide 60mg OD.
10 days ago he visited hospital for pain abdomen in the epigastric region, not associated with vomitings.
One week ago he had vomiting 3 episodes per day for 2 days, it was non projectile, non bilious with food particles as contents and non foul smelling.
There was yellowish discolouration of eyes.
From 4 days, patient developed abdominal distension, it was insidious in onset, gradually progressive.
It was not associated with pain abdomen, loose stools, fever.
From 2 days patient lost his appetite and is not passing stools.
From last night patient developed fever.
No H/O cough, cold
No H/O Hematemesis
No H/O pruritis
No H/O oliguria, hematuria
No H/O weight loss
HISTORY OF PAST ILLNESS:
• There is no history of similar complaints in the past.
• He is not a known case of HTN, ASTHMA,TB, EPILEPSY,CAD
• No history of blood tranfusions, surgeries in the past.
PERSONAL HISTORY:
Appetite- reduced
Diet -mixed
Sleep - disturbed
Bowel and bladder - no bowel movements, bladder regular
Duration of alcohol consumption unknown, increase in intake since 5 years- one quarter a day.
FAMILY HISTORY:
No similar complaints in the family.
No significant family history.
GENERAL EXAMINATION:
Consent of the patient taken.
He is moderately built and nourished.
• Pallor- absent
• Icterus - present
• Clubbing - absent
• Cyanosis - absent
• Lymphadenopathy - absent
• Edema - absent
VITALS
Temp : 99 F
PR : 80 bpm
RR : 15 cpm.
BP : 110/70 mm Hg
Spo2 : 98 %@ RA
SYSTEMIC EXAMINATION:
ABDOMEN EXAMINATION
INSPECTION:
Shape – elliptical
Flanks – full
Umbilicus –everted
All quadrants of abdomen are moving with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Percussion of liver for liver span
Percussion of spleen- dull note
AUSCULTATION:
Bowel sounds are feeble.
CARDIOVASCULAR SYSTEM
INSPECTION:
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse and pulsations cannot be appreciated
PALPATION:
Apical impulse is felt on the left 5th intercoastal space 2cm away from the midline.
No parasternal heave, thrills felt.
PERCUSSION:
Right and left heart borders percussed.
AUSCULTATION:
S1 and S2 heard , no added thrills and murmurs heard.
RESPIRATORY SYSTEM
INSPECTION:
Chest is bilaterally symmetrical
Trachea – midline in position.
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper/mid/lower interscapular were all RESONANT.
AUSCULTATION:
Normal vesicular breath sounds heard
No adventitious sounds heard.
CENTRAL NERVOUS SYSTEM EXAMINATION.
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
Right. Left
BULK
Upper limbs. N. N
Lower limbs N. N
TONE
Upper limbs. N. N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present , normal
Gait is normal
No involuntary movements
Sensory system - all sensations ( pain, touch, temperature, position, vibration sense) are
well appreciated .
INVESTIGATIONS:
Hemogram:
Blood grouping and RH typing:
INR: 1.8
Liver function tests:
21/3/22 21/3/22
Serum electrolytes
Ascitic fluid analysis
ABG
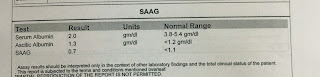
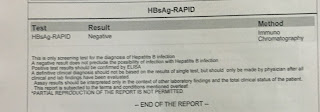
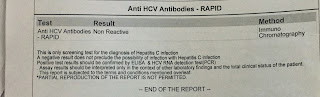
SEROLOGY
ECG
PROVISIONAL DIAGNOSIS:
Hepatic encephalopathy with alcoholic liver disease.
TREATMENT:
INJ. MONOCEF 2g IV BD
INJ. PAN 40 IV OD
T.RIFAGUT 550mg RT BD
SYP. LACTULOSE 10ml PO TID
TAB. URSODEOXYCHOLIC ACID 300mg PO BD
SYP. HEPAMEZ PO 10ml BD
INJ VITAMIN K 10mg over 10min.
• Tab. Atarax - 10mg PO OD.
• Physiogel lotion - local application BD.
























Comments
Post a Comment