FAMILY HISTORY:
He is a 4th order child ,born out of grade 4 consanguinous marriage.
He had one elder sister - who expired at 5 years of age.
He has 2 elders brothers.
His sister was the first child.
She was asymoptomatic till 2 years of age ,then she developed shortness of breath and was rushed to hospital,where here condition detiorated and had to be admitted.
She was diagnosed to have splenomegaly and her blood counts were decreasing.
She was given multiple blood transfusions, every 25 days,for one year- but remained anemic.
She also underwent bone marrow biopsy twice .
According to parents she was given steriods for one year before her death.
She never had jaundice or recurrent infections.
Eldest brother is 19 year old and second brother is 16.
Second brother had history of fever and white coloured loose stools at the age of 5 years , for which he was taken to the Nalgonda hospital.
He recovered on medication.
He was also diagnosed with anemia from which he recovered with some medications.
No history of Jaundice in this brother.
GENERAL EXAMINATION:
Consent of the patient taken.
The patient is conscious,coherent and cooperative; well oriented to time,place and person.
He is sitting comfortably on the bed.
He is lean build and moderately nourished.
• Height - 156cm
• Weight - 32kgs
• Pallor- present
• Icterus - present
• Clubbing - absent
• Cyanosis - absent
• Lymphadenopathy - absent
• Edema - absent
He has scars from his recent Chickenpox infection on limbs and trunk.
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse and pulsations cannot be appreciated
PALPATION:
Apical impulse is felt on the left 5th intercoastal space 2cm away from the midline.
No parasternal heave, thrills felt.
PERCUSSION:
Right and left heart borders percussed.
AUSCULTATION:
S1 and S2 heard , no added thrills and murmurs heard.
RESPIRATORY SYSTEM
INSPECTION:
Chest is bilaterally symmetrical
Trachea – midline in position.
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper/mid/lower interscapular were all RESONANT.
AUSCULTATION:
Normal vesicular breath sounds heard
No adventitious sounds heard.
ABDOMEN EXAMINATION
INSPECTION:
Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving with respiration.
No dilated veins, hernial orifices , sinuses
No visible pulsations
PALPATION:
Soft, non tender
Spleen:
A non-tender swelling is palpable in the left Hypochondrium enlarging towards the Right Iliac Fossa , it moves with respiration
The swelling is firm in consistency with a smooth surface and a rounded edge
Liver and Kidney are not palpable.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Enlarged spleen is dull on percussion.
AUSCULTATION:
Bowel sounds are heard.
CENTRAL NERVOUS SYSTEM EXAMINATION.
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
Right. Left
BULK
Upper limbs. N. N
Lower limbs N. N
TONE
Upper limbs. N. N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present , normal
Gait is normal
No involuntary movements
Sensory system - all sensations ( pain, touch, temperature, position, vibration sense) are
well appreciated .
INVESTIGATIONS:
Investigations ordered are : ECG, Hemogram, Bleeding and clotting time, prothrombin time, APTT, Urine analysis, Serology, USG - Abdomen.
Hemogram:
• There is significant drop in hemoglobin- from 8.9 to recent Hb -5 units.
• Leucopenia.
Hemoglobin electrophoresis:
Blood grouping and RH typing:
Bleeding and Clotting time:
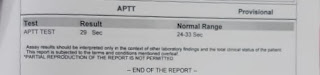
APTT :
Liver function tests:
Sr.CR- 0.7
urea-17
Na+- 141
k+-4
cl- 97
Thyroid profile:
T3-61
T4- 8.66
TSH- 91.85
ANTI TPO ANTIBODIES- 771.1
Direct Coomb’s test- POSITIVE
Stool for occult blood- Negative
USG abdomen:
Splenomegaly seen.

ECG:
PROVISIONAL DIAGNOSIS:
• Thyroditis
• Spectrum of Autoimmune diseases.
• Autoimmune Hemolytic Anemia.
• Chronic itching of both hands and limbs - suggests CVID (common variable immunodeficiency).
TREATMENT:
• Tab. Thyronorm - 200mg PO OD.
• Tab. Methylprednisolone - 32mg PO OD.
• Tab. Atarax - 10mg PO OD.
• Physiogel lotion - local application BD.
The patient is now under observation.

















Comments
Post a Comment