SUDHAMSHI REDDY M
MBBS 9th semester
Roll no:80
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
A 74 yr old male, resident of Narketpally presented to the casuality with chief complaints of
- Fever since 3 days
- Decreased urine output since 2 days
- SOB :Grade 3 since 1 day
HISTORY OF PRESENTING ILLNESS :
1.FEVER:
- Sudden in onset, associated with chills,
increased during night time and it relieved on
taking medication.
- 2 days ago the patient was connected to urine
bag, this increased fever.
2.DECREASED URINE OUTPUT:
- Normal frequency 4 times/day and 3 times/
nighttimes.
- Since 2 days from tuesday morning, output
decreased.
- went to local RMP on Tuesday night at night
10pm and urine bag was connected.
3.SOB GRADE : 3
- Present while walking & at rest also.
PAST HISTORY :
- Patient was apparently asymptomatic 2 months back, then he was admitted in our
hospital and diagnosed with
- left facial nerve palsy, peripheral neuropathy(? ATT INDUCED)
- denovo HTN (? post pulmo tb)
- Spondyloarthropathy with radiculopathy sacroileitis cervical OPLL ( Ossification of posterior longitudinal ligament) - Ankylosing spondylitis
- Known case of DM - 2 since 20 yrs
PERSONAL HISTORY:
Diet: vegetarian
Appetite: decreased since 1 month
Sleep: decreased since 2 days
Bowel and bladder movements: urine decreased
Addictions: smoking present since 20 yrs ( 3 packets/day ) stopped 5 yrs back
GENERAL EXAMINATION:
The patient is examined in a well lit room, with informed consent.
Pallor : absent
Icterus : absent
Cyanosis : absent
Clubbing : absent
Lymphadenopathy : absent
Edema : absent
SYSTEMIC EXAMINATION:
CVS: S1 and S2 heard
No added thrills, murmurs
RESPIRATORY SYSTEM: Normal vesicular breath sounds heard, position of trachea central,
no adventitious sounds heard, no dyspnea and wheeze.
PER ABDOMEN: Soft,tenderness & pain present
abdominal distention: present
CENTRAL NERVOUS SYSTEM: FNAD
PROVISIONAL DIAGNOSIS:
- AKI (Prerenal/Renal)ON CKD k/c/o HTN/DM cervical spondylosis, ankylosing
spondylosis.
-Altered sensorium secondary to metabolic (? Hepatic/uremic)
TREATMENT :
DAY : 0
1.IVF NS & RL @ 100ML/HR
2.INJ PIPTAZ 4.5 gm IV STAT
INJ PIPTAZ 2.25GM IV TID
1_______X________1
3.INJ PAN 40 MG IV OD
8AM _____X
4.INJ ZOFER 4MG/IV/SOS
5.INJ PCM 1GM IV SOS(IF TEMP >101°F)
6.INJ NORAD INFUSION( 2 AMP IN 46ML NS) @ 8ML/HR
7.BP CHARTING 2ND HRLY
8.TEMP/PR/BP CHARTING 2ND HRLY
9.INJ HAI SC (8AM__1PM___8PM)
10.GRBS CHARTING 6TH HRLY
( 8AM__1PM___8PM__2AM)
NEPHRO REFERRAL
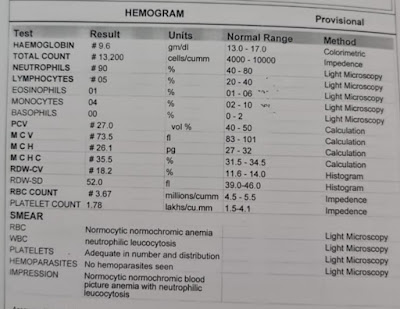
HEMOGRAM
RBS
LFT
SERUM ELECTROLYTES
SERUM CREATININE
BLOOD UREA
2D ECHO
ABG
CHEST X RAY
ECG AT 7:45 PM
AT 10:40 PM
AT 12:40 AM
DEATH SUMMARY:
A 70 yr old male, came to casualty with c/o SOB :1 DAY(GRADE 2 - 3) with pulse not palpable, BP not recordable.ABG showing metabolic acidosis.Bicarbonate correction was given.Fluid resuscitation was planned. Triple lumen catheter ionotropic support was started with noradrenaline, dobutamine titrated to requirement.Nephrology opinion was taken i/v/o increased urea & creatinine, dialysis was advised around 7 pm. CPR was initiated, Pt revived ABG showing severe metabolic acidosis.ventilator settings MODE: ACMV- VC, FiO2: 100%, PEEP: 5 cm H2O, V : 50 ml.Around 1:25AM pt became unresponsive.BP not recordable, pulse not palpable, CPR was initiated according to AHA guidelines. Despite the above resuscitation efforts, pt could not be revived & declared dead on 22/10/21 @ 2:01AM
IMMEDIATE CAUSE: - Refractory hypotension, metabolic acidosis with type 1 respiratory failure
ANTECEDENT CAUSE:
- AKI(intrinsic) on CKD with metabolic encephalopathy (?Hepatic/uremic) post CPR status k/c/o T2 DM & HTN















Comments
Post a Comment