MEDICINE BLENDED BIMONTHLY ASSIGNMENT -MAY 2021
CASE 1 PULMONOLOGY
A 55 year old female with shortness of breath, pedal edema and facial puffiness.
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
Efficacy based on studies: Moderate quality evidence from eight studies involving 759 participants demonstrated that a semi-recumbent (30º to 60º) position reduced clinically suspected VAP by 25.7% when compared to a 0° to 10° supine position.
➣O2 inhalation-
- Indication for o2 inhalation: supplemental o2 therapy / inhalation is given when spo2
levels are < 92% at room air.
➣Intermittent BiPAP-
- MOA:
because it helps to open lungs with this air.
The machine has 2 pressure settings:
1) for inhalation IPAP
2) low pressure foe exhalation EPAP
-It is given to the patient to treat Broncheictasis
-Augmentin is a combination of-
AMOXICILLIN- binds to penicillin binding proteins in bacterial cell wall and thereby
inhibits bacterial cell wall synthesis.
CLAVULINIC ACID- is a beta lactamase enzyme inhibitor, thereby facilitates action of
Amoxicillin.
-It is given to the patient to provide symptomatic relief and reduce incidence of acute
EFFICACY BASED ON A STUDY:
A randomized controlled trial found that patients hospitalized for an acute exacerbation
of chronic obstructive pulmonary disease (COPD) experienced reduced rates of treatment
failure when adding azithromycin to their standard of care.
During the study, patients received a low dose of azithromycin in addition to their prescribed
medications while in the hospital and continued taking the antibiotic for 3 months following hospitalization. The result, according to the data, was reduced treatment failure compared
with standard of care alone. Rates of treatment failure were under 50% for patients taking azithromycin (49%) compared with 60% for patients receiving standard of care.
-It is given to the patient to relieve symptoms of fluid retention(edema)
-It is also used to treat hypertension.
Furosemide(LASIK) acts by inhibiting the luminal Na-K-Cl cotransporter in the thick
ascending limb of loop of Henle.
⬇️
Increases the excretion of Na+ and water by the kidneys
⬇️
Increases urine output
- It acts by reducing inflammation in the body
-Based on a study…In comparison to placebo, systemic corticosteroids
- improved airflow,
- decreased the rate of treatment failure and risk of relapse
- improved symptoms and decreased the length of hospital stay
-Budecort (Budesonide ) belongs to a group of medicines called 'corticosteroids'. It works
by reducing and preventing swelling and inflammation in your lungs’.
Efficacy based on a study where Patients received 2 mg of budesonide every 6 h
(n = 71placebo (n = 66). All received standard treatment, including nebulized
beta(2)-agonists, ipratropium bromide, oral antibiotics, and supplemental oxygen.
The mean change (95% confidence interval) in postbronchodilator FEV(1) was greater
with active treatments than with placebo: budesonide versus placebo, 0.10 L (0.02 to 0.18 L)
➣TAB Pulmoclear 100 mg PO OD
-Pulmoclear Tablet is a combination of two mucolytic medicines:
Acebrophylline
Acetylcysteine.
It thins and loosens mucus (phlegm) making it easier to cough
It also relaxes the airway muscles and thereby promotes easy inflow and outflow of air
➣Chest physiotherapy
Chest physiotherapy improves lung function ,expands the lungs, strengthens breathing
muscles, loosens and improves drainage of thick lung secretions.
➣GRBS 6 hrly - to monitor blood sugar levels
➣INJ. HAI SC ( 8 am- 2pm- 8pm)
Human Actrapid Injection contains human insulin(short acting)
It is given to the patient to lower blood sugar levels as she is a diabetic.
➣Temp, BP, PR, SPO2 monitoring
➣I/O charting - Is used to record fluid intake and output
➣INJ. THIAMINE 1 amp in 100 ml of NS
Based on a study- The administration of a single dose of thiamine was associated with a
trend toward increase in oxygen consumption in critically ill patients.
-Thiamine deficieny is seen in patients taking loop diuretics(LASIK), as this patient is
receiving LASIK, the use of thiamine could be prophylactic.
➤ Anatomical localisation - CENTRAL NERVOUS SYSTEM.
➤ Etiology - Patient has a history of alcohol consumption.
Excess consumption of alcohol leads to deficieny of Thiamine, this gives rise to a
condition known as Wernicke's Encephalopathy.
-Human Actrapid Injection contains human insulin(short acting)
- It is used to control blood sugar levels.
➣ IVF NS and RL @150ml/hr
-Normal saline and ringer lactate solutions are both crystalloid fluids.
-NS contains 154 mM Na+ and Cl-, with an average pH of 5.0 and osmolarity of
308 mOsm/L.
- LR solution has average pH of 6.5, is hypo-osmolar (272 mOsm/L), and has similar
electrolytes (130 mM Na+, 109 mM Cl-, 28 mM lactate, etc.).
- This is given to the patient to maintain fluid levels.
➣ Inj 2 ampoule KCl (40mEq) in 10 NS over 4 hours
- Supplemental potassium is used as an electrolyte replensher, treats hypokalemia.
➣ Syp Potchlor 10ml in one glass water/PO/BD
- Is a supplement of potassium.
3. Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
Ans : Patient has two main neurological symptoms-
. Seizures
. Memory loss
-Seizures- this could be due to a process known as KINDLING.
Repeated consumption and withdrawal of alcohol is known as Kindling. This results
in electrical and chemical stimulation and can precipitate seizure activity.
-Memory loss- continuous use of alcohol results in thiamine deficiency - this leads to
widespread cerebral and subcortical atrophy.
4. What is the reason for giving thiamine in this patient?
5. What is the probable reason for kidney injury in this patient?
Ans : Alcohol induced kidney injury-
The kidneys have an important job as a filter for harmful substances.
- Alcohol causes changes in the function of the kidneys and makes them less able to
filter the blood.
-Alcohol also affects the ability to regulate fluid and electrolytes in the body.
-When alcohol dehydrates the body, the drying can affect the normal
function of all cells and organs, including the kidneys.
- Alcohol also disrupts hormones this in turn affects kidney function.
- Chronic drinking affects the liver. The rate of blood flow to the kidney is maintained by
liver , therefore liver disease disrupts this balance and affects the kidney function.).
6. What is the probable cause for the normocytic anemia?
Ans : The probable cause for normocytic anemia in this patient is kidney disease.
7. Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
Ans : Yes , chronic alcoholism could have aggravated the formation on the foot ulcer.
In the case of a chronic alcoholic, there is a depression in the immune system, as seen is
diabetics.
Chronic alcoholism can also lead to alcoholic neuropathy.
Alcoholic neuropathy involves coasting caused by damage to nerves that results
from long term excessive drinking of alcohol . Chronic presentation will increase the
chances of foot ulcer formation and also increase the time of recovery.
CASE 2
A 52 year old male with cerebellar ataxia.
https://kausalyavarma.
Ans :
➤ Timeline of events :
7 DAYS AGO - An episode of giddiness that started around 7 in the morning, subsided on
taking rest, was associated with vomiting.
↓
4 DAYS AGO - An episode of giddiness following alcohol consumption.
It was sudden in onset, continuous and gradually progressive, increased on
standing and while walking.
- Bilateral hearing loss, aural fullness, tinnitus.
- 2-3 episodes of vomiting, non projectile and non bilious.
↓
DAY OF ADMISSION - Slurring of speech and deviation of mouth.
➤ Anatomical localisation : CENTRAL NERVOUS SYSTEM( cerebellum)
➤ Etiology : The above symptoms point out to the involvement of cerebellum.
Ataxia is the lack of coordination of voluntary movements such as walking.
In this case the patient is a hypertensive, is not taking the prescribed
medications. This increases the risk of clot formation in the brain, this results
in reduced blood supply to the brain( stroke) can thereby
result in ataxia.
Ans : Following are the interventions used for this patient.
➣Tab Veratin 8 mg PO TID
- Vertin is a betahistine, an anti vertigo medication.
- MOA : It is a weak agonist on H1 receptors located on blood vessels of inner ear. This
leads to vasodilatation and increases vascualr permeability.
- Indication : Used to treat balance disorders.
➣Inj Zofer 4 mg IV/TID
- Zofer is an antimetic medication.
- MOA : It is a 5H3 receptor antagonist on vagal afferents in the gut , blocks receptors even
in CTZ .
- Indication : it is given to this patient to control the episodes of nausea and vomiting.
➣Tab Atorvostatin 40 mg PO/HS
➣ Tab Clopidogrel 75 mg PO/OD
- Clopidogrel is an antiplatelet medication.
- MOA : It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on
the platelets.
- It is given to this patient to reduce the risk of further clot formations.
➣ Tab Ecospirin 75mg-
- Ecospirin is an anti inflammatory and antiplatelet medication.
- It is given to the this to prevent further clot formation.
➣ Inj Thiamine 1 AMP in 100 ml NSPO/BD
- It is given to the patient to combat its deficiency as he is a chronic alcoholic.
3. Did the patients history of denovo HTN contribute to his current condition?
High blood pressure increases stress on blood vessels , impairs adaptive responses.
By this mechanism high BP increases the risk.
4. Does the patients history of alcoholism make him more susceptible to ischaemic or
haemorrhagic type of stroke?
Ans :
CASE 3
A 45 year old female patient with palpitations, pedal edema , chest pain, chest haeviness, radiating pain along left upper limb.
http://bejugamomnivasguptha.
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans :
➤ Timeline of events :
10 YEARS AGO - An episode of right and left upper limb paralysis.
↓
1 YEAR AGO - An episode of right and left paresis due to Hypokalemia.
↓
8 MONTHS AGO - Bilateral pedal edema, gradually progressive, present in both sitting
and standing position, relieved on medication.
↓
7 MONTHS AGO - Diagnosed with blood infection
↓
2 MONTHS AGO - Patient had neck pain , received treatment at the hospital.
↓
6 DAYS AGO - Pain in the left upper limb, dragging type, pain increased in the night,
aggravated during palpatations and relieved on medication.
↓
5 DAYS AGO - Palpitations , sudden in onset, more durimg the night, aggravated by lifting
weights and speaking continuously, relieved on medication.
- Grade 3 SOB during episodes of palpitations.
- Chest pain associated with chest heaviness
➤ Anatomical localisation : Cervical spine
➤ Etiology : The episodes of chest pain, palpitations, paresis, edema experienced by the
patient could be due to Hypokalemia.
Neck pain experienced by the patient could be due to Cervical spondylosis.
Ans : The reasons for recurrence of Hypokalemia in this patient are:
. Diuretics use
. Albumin is completely absent in this patient- indicating severe malnutrition,
inflammation, this can result in Hypokalemia.
- The risk factors for hypokalemia include :
Malnutrition
.Use of diuretics
.Diarrhoea
.Vomitings
. Excessive alcohol use
. Excessive sweating.
3. What are the changes seen in ECG in case of hypokalemia and associated symptoms?
Ans : The earliest electrocardiogram (ECG) change associated with hypokalemia is a
decrease in the T-wave amplitude. As potassium levels decline further, ST-segment
depression and T-wave inversions are seen, while the PR interval can be prolonged
along with an increase in the amplitude of the P wave.
Appearance of U wave in the mid precordial leads.
CASE 4
A 55 year old male with seizures.
https://rishikoundinya.
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Ans : -Stroke is the most common cause of seizures in the elderly.
- Stroke is of two types:
.Hemorrhagic stroke- this occurs as a result of bleeding within or around the brain.
. Ischemic stroke- this occurs as a result of blood clot or a lack of blood flow to the
brain.
Hemorrhagic stroke increases the risk of seizures than an ischemic stroke. There is also increased risk of seizures if the stroke is severe or occurs within the cerebral cortex of your brain.
Seizures following a stroke( post seizure stroke) are of 2 types:
-Early onset seizures have peak within 24 hours after stroke.
-Late onset seizures occur after 2 week of stroke onset, peak within 6-12 months after
the stroke , has a higher rate of recurrence.
-EPILEPSY- is a condition characterised by recurrent episodes of seizures
PATHOGENESIS OF SEIZURES FOLLOWING STROKE-
Early onset seizures after ischaemic strokes are due to :
An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for
depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction,
destruction of phospholipid membrane, secretion of free fatty acids in penumbral areas.
↓
- Late onset seizures are due to glottic scarring and are associated with the persistent
changes in neuronal excitability.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Ans : The patient has a history with seizure activity, so due to this there is an increase in the
chemical and mechanical activity , which leads to the development of organic lesions in
the brain.
The bigger the lesions the more severe the symptoms.
Since this patient has had recurrent seizures (15episodes in the last 5 years) there
might be an aggravation of symptoms during this episode compared to the last.This
could be responsible for his loss of consciousness.
CASE 5
A 48 year old male with seizures and altered sensorium.
A potential mechanism for this is alteration in GABA-A receptor dependent
neurotransmission. Ethanol is shown to disrupt molecular events at the mossy fibre-
granule cell-golgi cell synaptic site and the granule cell fibre-Purkinje cell synaptic site,
Ethanol also causes neuroinflammation and neurotoxicity in the cerebellum.
All these affect the cerebellum, which is the motor coordination centre of the central
nervous system, and also involved in cognitive processing and sensory discrimination.
These can all result in altered hand movements, impaired postural stability and balance, loss of fine movements etc.
Bleeding diathesis is an unusual susceptibility to bleed (hemorrhage) mainly due to
hyper coagulability. Heavy drinking can cause thrombocytopenia, as well as impact
and functions of platelets. Impaired platelet function, together with reduced platelet
count, can contribute to this condition associated with chronic alcoholism.
In the above study, RTA led to a delayed infarct formation( 5 weeks following
accident).
Similarly, the accident that occurred in our patient 4 years ago could be the reason for his
present condition.
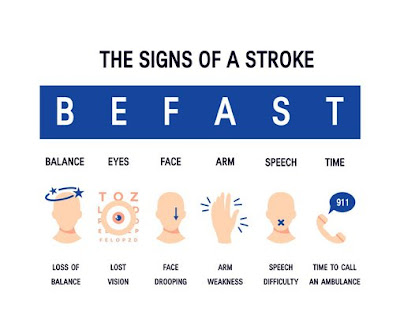
2.What are warning signs of CVA?
Ans : The warning signs of CVA include -
• Sudden numbness or weakness in the face, arm, or leg, especially on one side of the
body.
• Sudden confusion, trouble speaking, or difficulty understanding speech.
• Sudden trouble seeing in one or both eyes.
• Sudden trouble walking, dizziness, loss of balance, or lack of coordination.
• Sudden severe headache with no known cause.
- According to the above study, patients who consume 1-21 drinks a week, have a lower
chance of developing ischemic or hemorrhagic stroke than those who are heavy
drinkers. The patient is an occasional alcohol drinker, so the chances of alcohol
affecting his attack is improbable. In heavy drinkers, alcohol can increase the chances
of both types of strokes.
5.Does his lipid profile has any role for his attack?
Ans : Lipid profile of the patient is overall normal except HDL count.
HDL level in the patient is 33mg/dl which is lower than the normal range (40-60 mg/dl).
-Studies have demonstrated a trend toward a higher risk of stroke with lower HDL-C.
HDL-C is considered as an important modifiable stroke risk factor. In patients with
recent stroke or transient ischemic attack and no coronary heart disease, only lower
baseline HDL-C predicted the risk of recurrent stroke.
CASE 7
A 50 year old male with cervical myelopathy.
https://amishajaiswal03eloggm.blogspot.com/2021/05/a-50-year-old-patient-with-cervical.html
1.What is myelopathy hand?
-when patient holds fingers extended and adducted, the small finger spontaneously
abducts due to weakness of intrinsic muscle.
-It is a component of Wartenberg’s sign-consisting of involuntary abduction of the fifth
(little) finger, caused by unopposed action of the extensor digiti minimi. This
commonly results from weakness of the ulnar nerve innervated intrinsic hand muscles
particularly PALMAR INTEROSSEOUS MUSCLE .
3.What is Hoffman’s reflex?
Ans : Also known as DIGITAL reflex, SNAPPING reflex, JACOBSON’S reflex.
.It is used to examine the reflexes of upper extremities.
PROCEDURE— The doctor carries out the test procedure by:
holding the middle finger at the joint closest to the fingernail, flicks the nail using the
other hand.
INTERPRETATION-
. If there is no movement in the index finger or thumb after this motion, the person has
a negative Hoffman’s sign.
. If the index finger and thumb move, the person has a positive Hoffman’s sign.
A positive Hoffman sign indicates an upper motor neuron lesion and corticospinal
pathway dysfunction likely due to cervical cord compression. (Eg: CERVICAL
MYELOPATHY). However, a positive Hoffman sign can be present in an entirely
normal patient. This happens in individuals who are hyper reflexive.
CASE 8
A 17 year old female with seizures
.https://neerajareddysingur.blogspot.com/2021/05/general-medicine-case-discussion.html?m=1
1. What can be the cause of her condition ?
Ans : The patient’s GTCS episodes can be due to acute cortical vein thrombosis as seen in her
MRI.
Seizures are the most common symptoms of CVT.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5771304/
This case report illustrates that CVT can occur in the presence of anaemia and
thrombocytopenia.
The above case is similar to this patient. This illustrates that iron deficiency anemia and
thrombocytopenia can alone be considered as risk factors for CVT.
2. What are the risk factors for cortical vein thrombosis?
Ans : The risk factors for CVT are as follows -
- Excessive use of birth control pills.
- Head injury
- Protein deficiencies
- Obesity
- Ear, neck, face infections.
- Dehydration
- Chronic hemolytic anemia.
-HF with preserved ejection fraction, ( HFpEF) Also known as diastolic HF.
- In HFpEF, the muscles of the heart contract normally and the heart may seem to pump a
normal proportion of the blood that enters it. However, heart muscle thickening may
cause the ventricle to hold an abnormally small volume of blood( chamber hypertrophy)
Therefore, although the heart’s output may still appear to be in the normal range, its
limited capacity is inadequate to meet the body’s requirements.
Causes-CORONARY ARTERY DISEASE, HYPERTROPHIC CARDIOMYOPATHY,
AORTIC STENOSIS, HIGH BLOOD PRESSURE
-HF with reduced ejection fraction (HFrEF), also known as systolic HF,.
In this, the heart muscle is not able to contract adequately( chamber dilatation) and
therefore, expels less oxygen-rich blood into the body. Patients with this form of the
disease will have lower-than-normal left ventricular ejection fraction on an
echocardiogram.
Causes- Diabetes, Hypertension, valvular heart disease
LVEF of 50% to 75% indicates a normal pumping ability
36% to 49% is considered below normal
35% or lower is considered low pumping ability.
-Fatigue and shortness of breath are common symptoms of both HFpEF and HFrEF.
2.Why haven't we done pericardiocenetis in this pateint?
Ans :Pericardiocentesis is a procedure done to remove fluid that has built up in the sac
around the heart (pericardium).
It's done using a needle and small catheter to drain excess fluid.
-There are 3 approaches for needle entry - left parasternal, subxyphiod approach, left
apical approach.
All these require a lot of precision as they might damage the surrounding pleura,
diaphragm, liver.
. Pericardial effusion is mild - moderate in this patient , so symptomatic treatment was
given rather than opting for an invasive procedure like pericardiocentesis which requires
a lot of precision.
. Also this patient has pleural effusion, this might make fluid extraction difficult without
inflicting any damage as the needle is inserted very close to the pleura.
.MECHANISM
Cigarette smoking leads to impaired endothelial function via decreased nitric oxide
production, pro-thrombotic state, increased oxidative stress, and activated inflammatory
pathways.
In addition to vascular effects, smoking, via increased oxidative stress and inflammation
directly effects on the myocardium leading to systolic and diastolic dysfunction.
It also promotes other heart failure (HF) risk factors including blood pressure, increased
heart rate, diabetes, and atherosclerosis.
BASED ON STUDIES- We have recently seenD that smoking is independently
associated with 5-year risk for HF in older adults.
B) Chronic alcoholic ( 90ml per day for the past 30 years)
Heavy alcohol consumption is associated with alcoholic cardiomyopathy
- Alcoholic cardiomyopathy is characterized by left ventricular dilation, increased left
ventricular mass, and reduced or normal left ventricular wall thickness among patients
with a long-term history of heavy alcohol consumption (5-15 years). -
-Based on studies alcoholic patients with symptomatic HF had 10 years or more of
exposure to heavy drinking .
All these indicate risk of HF in a chronic alcoholic.
C) Hypertension and Diabetes
Diabetes results in changes in myocardial structure and function.
- Disproportionate left ventricular hypertrophy
- Perivascular and interstitial fibrosis
These changes stiffen the heart , will result in diastolic and systolic dysfunction and
increase risk of heart failure.
Hypertension increases work load on the heart and a result there is left ventricular
hypertrophy — risk of heart failure
D)ECG reports of the patient indicate first degree AV block.
This is associated with an increased risk of heart failure.
Among patients with heart failure, first-degree atrioventricular block is present in anywhere
between 15% and 51%.
E) 2D ECHO of the patient shows pericardial effusion
This increases pressure on the heart and if left untreated will lead to heart failure.
4.What could be the cause for hypotension in this patient?
Ans :Hypotension in this patient could be due to combination of pericardial effusion and use
of diuretic LASIX.
The pumping ability of the heart in this patient is compromised , along with this he is
on Diuretic and anti hypertensive ( Telma 40 mg) , fluid restriction- all this might result
in Hypovolemia and thereby Hypotension.
CASE 2
A 73 year old male with pedal edema, shortness of breath and decreased urine output.
https://muskaangoyal.blogspot.com/2021/05/a-73-year-old-male-patient-with-pedal.html
1.What are the possible causes for heart failure in this patient?
Ans : The patient has various comorbidities which could have led to a heart failure:
1.He is a chronic alcoholic since 40 years which is a risk factor towards heart failure
https://www.nmcd-journal.com/article/S0939-4753(19)30360-6/fulltext
The findings in this article provide longitudinal evidence that moderate and heavy
alcohol consumption are associated with decreased LVEF and trend towards a higher
risk of incident LV systolic dysfunction, compared to light drinkers.
2. Patient was diagnosed with type 2 diabetes mellitus 30 years ago and has been
taking human mixtrad insulin daily and was also diagnosed with diabetic triopathy
indicating uncontrolled diabetes which is considered to be a major risk factor for heart
failure.
3. The patient was diagnosed with hypertension 19 yrs ago which is also considered as
a risk factor for heart failure.
4. The patient has elevated creatinine and AST/ALT ratios is >2 and was diagnosed with
chronic kidney disease stage IV. CKD is also one of the risk factors for heart failure.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2900793/
Chronic kidney disease results in decreased production of erythropoietin which in turn
decreases the production of red blood cells from the bone marrow.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
Ans :The main reason for blebs and non-healing ulcer in this patient is uncontrolled diabetes
mellitus. CKD is also known to cause delay in healing of wounds along with poorly
controlled diabetes.
- insulin resistance
- prediabetes
- type 2 diabetes and
- type 2 diabetes and vascular complications, including retinopathy, nephropathy or neuropathy and, or, related microvascular events.
Congestive heart failure is a chronic progressive condition that affects the
pumping power of the cardiac muscle. It occurs if the heart cannot pump
(systolic) or fill (diastolic) adequately. Loss of atrial contraction and left atrial
dilation in this case cause stasis of blood in the left atrium and may lead to
thrombus formation in the left atrial appendage. This predisposes to stroke and
other forms of systemic embolism.
➣ TAB. Cardivas 3.125mg PO/BD-
- MOA- It is carvediol. It blocks B1, B2, Alpha 1 adrenergic receptors and no
intrinsic sympathomimetic activity.
- Indications- Used as a long term drug to reduce mortality in patients with
congestive heart failure.
➣ TAB. Dytor 10mg PO/OD-
-MOA- It is torsemide, a loop high ceiling diuretic. It acts on the thick ascending
limb of the loop of henle, increases Na, K and Cl excretion in the urine.
-Indications- preferred in cases of hypertension associated with CCF and renal failure.
➣ TAB Pan D 40mg PO/OD -
-MOA- It is a combination of domperidone and pantaprazol. It is a proton pump
inhibitor and helps decrease acid production in the stomach.
-Indications- used to treat gastroesophageal reflux disease (Acid reflux) and peptic
ulcer disease by relieving the symptoms of acidity such as indigestion, heartburn,
stomach pain, or irritation.
➣TAB. Taxim 200mg PO/OD-
- MOA- It is cefixime. They are beta-lactam antibiotics that inhibit synthesis of
bacterial cell wall and produce a bactericidal effect.
-Indications- Given mainly to prevent development of bacterial infections.
a) Patient has Diabetes mellitus type 2, which can accelerate atherosclerosis by driving
inflammation and slowing down blood flow.
b) Patient has history of alcohol abuse that can lead to atherosclerosis and increase the
risk of stroke.
c) Patient has a history of NSAID abuse, which can change the vessels ability to relax
and also stimulate growth of smooth muscle cells inside the arteries, thus leading to the
clogging of the arteries.
d) Patient also has a history of hypertension- effect on the arterial wall also results in the
aggravation and acceleration of atherosclerosis, particularly of the coronary and cerebral
vessels. Moreover, hypertension appears to increase the susceptibility of the small and
large arteries to atherosclerosis.
INR- It is international normalized ratio; it is also a measure of the ability of the blood to
clot. This is an important test for patients who are on blood thinners (ie) anticoagulants
The patient in this case was taking heparin, so it is necessary to monitor this ratio.
CASE 4
Pharmacological interventions:
➣TAB MET XL 25 MG/STAT-
-contains Metoprolol as active ingredient
-MOA: METOPROLOL is a cardioselective beta blocker.
Beta blockers work by blocking the effects of the hormone epinephrine, also known
as adrenaline. Beta blockers cause your heart to beat more slowly
( negative chronotropic effect) and with less force( negative inotropic effect).
Beta blockers also help open up your veins and arteries to improve blood flow.
-Indications: it is used to treat Angina, High blood pressure and to lower the risk of
heart attacks .
EFFICACY STUDIES:
Patients were randomized to one of four treatment arms: placebo or ER metoprolol (0.2 mg/kg, 1.0 mg/kg, or 2.0 mg/kg). Data were analyzed on 140 intent-to-treat patients.
Results: mean baseline BP was 132/78 +/- 9/9 mmHg. Following 4 weeks of treatment, mean changes in sitting BP were: placebo = -1.9/-2.1 mmHg; ER metoprolol 0.2 mg/kg = -5.2/-3.1 mmHg; 1.0 mg/kg = -7.7/-4.9 mmHg; 2.0 mg/kg = -6.3/-7.5 mmHg. Compared with placebo, ER metoprolol significantly reduced systolic blood pressure (SBP) at the 1.0 and 2.0 mg/kg dose (P = .027 and P = .049, respectively), reduced diastolic blood pressure (DBP) at the 2.0 mg/kg dose (P = .017), and showed a statistically significant dose response relationship for the placebo-corrected change in DBP from baseline. There were no serious adverse events or adverse events requiring study drug discontinuation among patients receiving active therapy.
➣Non pharmacological intervention advised to this patient is: PERCUTANEOUS
CORONARY INTERVENTION.
Percutaneous Coronary Intervention is a non-surgical procedure that uses a
catheter (a thin flexible tube) to place a small structure called a stent to open up
blood vessels in the heart that have been narrowed by plaque buildup
( atherosclerosis).
3. What are the indications and contraindications for PCI?
Ans : INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.
Absence of cardiac surgery backup.
Hypercoaguable state.
High-grade chronic kidney disease.
Chronic total occlusion of SVG.
An artery with a diameter of <1.5 mm.
4. What happens if a PCI is performed in a patient who does not need it? What are the harms
of overtreatment and why is research on overtesting and overtreatment important to current
healthcare systems?
Ans: Although PCI is generally a safe procedure, it might cause serious certain
complications like -
A)Bleeding
B) Blood vessel damage
C) Allergic reaction to the contrast dye used
D) Arrhythmias
E) Need for emergency coronary artery bypass grafting .
Because of all these complications it is better to avoid PCI in patients who do not
require it.
- OVER TESTING AND OVER TREATMENT HAVE BECOME COMMON IN TODAY’S MEDICAL PRACTICE.
- Research on overtesting and overtreatment is important as they are more harmful than useful.
Harms to patients
. Performing screening tests in patients with who at low risk for the disease which is being
screened.
For example:Breast Cancer Screenings Can Cause More Harm Than Good in Women
who Are at Low Risk. A harmless lump or bump could incorrectly come up as cancer
during routine breast screenings. This means that some women undergo surgery,
chemotherapy or radiation for cancer that was never there in the first place.
-Overuse of imaging techniques such as X- RAYS AND CT SCANS as a part of routine
investigations.
-Overuse of imaging can lead to a diagnosis of a condition that would have otherwise
remained irrelevant - OVERDIAGNOSIS.
Also the adverse effects due to this are more when compared to the benefits.
-Over diagnosis through over testing can psychologically harm the patient.
-Hospitalisations for those with chronic conditions who could be treated as outpatients
can lead to economic burden and a feeling of isolation.
Harms to health care systems
The use of expensive technologies and machineries are causing burden on
health care systems.
CASE 5
A 60 year old male with chief complaints of chest pain, giddiness and profuse sweating.
.https://bhavaniv.blogspot.com/2021/05/case-discussion-on-myocardial-infarction.html?m=1
➤Anatomical Localisation : CARDIOVASCULAR SYSTEM (Occlusion of the right
coronary artery)
➤ Etiology : The causes for the occlusion of right coronary artery can be-
• Atherosclerosis – Also known as coronary artery disease, this condition
is the most common cause of heart attacks and occurs when the buildup
of fat, cholesterol, and other substances forms plaque on the walls of the
coronary arteries.
• Coronary artery spasm
• Coronary artery tear
2. What are mechanism of action, indication and efficacy over placebo of each of the
pharmacological and non pharmacological interventions used for this patient?
Ans : Following interventions are used in this patient -
➣ TAB ATORVAS 80mg PO/STAT -
- MOA : Atorvastatin is a statin medication and a competitive inhibitor of the
enzyme HMG-CoA reductase, which catalyzes the conversion of HMG-CoA
to mevalonate, an early rate-limiting step in cholesterol biosynthesis.
Atorvastatin acts primarily in the liver, where decreased hepatic cholesterol
concentrations stimulate the upregulation of hepatic low-density lipoprotein
receptors, which increases hepatic uptake of LDL. Atorvastatin also reduces
Very-Low-Density Lipoprotein-Cholesterol, serum triglycerides and
Intermediate Density, but increases High-Density Lipoprotein Cholesterol.
- Indication : Atorvastatin is used for the treatment of several types of dyslipidemias.
- Atorvastatin can be used as a preventive agent for myocardial infarction,
stroke, and angina, in patients without coronary heart disease but with
multiple risk factors.
➣ TAB. ASPIRIN 325 mg PO/STAT -
-MOA : Aspirin is a NSAID. They inhibit COX-1 and COX-2 thus decreasing the
prostaglandin level and thromboxane synthesis.
-Indications : They are anti platelet medications and, in this case, used to prevent
formation of blood clots in blood vessels.
-Efficacy over Placebo: According to a study, Aspirin use was associated with a
lower risk of myocardial infarction when compared to a
placebo.
➣TAB CLOPIBB 300mg PO/STAT-
-MOA : Clopidogrel is an antiplatelet medication, it metabolised to its active form by
carboxylesterase-1. The active form is a platelet inhibitor that irreversibly
binds to P2Y12 ADP receptors on platelets. This binding prevents ADP
binding to P2Y12 receptors, activation of the glycoprotein GPIIb/IIIa complex
and platelet aggregation.
-Indications : Clopidogrel is indicated to reduce the risk of myocardial infarction for
patients with non-ST elevated acute coronary syndrome, patients with ST-
elevated myocardial infarction, and in recent MI, stroke.
➣ INJ HAI 6U/IV STAT - is given to control elevated blood sugar levels.
Though there are certain benefits from PTCA, there are some disadvantages too.
If done along with systemic thrombolytics then it can lead to a higher incidence of
bleeding complications.
Just PTCA alone, has not proven to show any ventricular function improvement or
decreased mortality.
CASE 6
A 87 year old male with shortness of breath, constipation and decreased urine output.
https://kattekolasathwik.
In cardiogenic shock, there is hypovolemia, this will reduce perfusion to major organs
in the body, when there is decreased perfusion, the body slows starts shutting down.
To halt this process, iv fluids are given rapidly to continue the perfusion of fluids at the
normal rate. This helped in relieving shortness of breath.
Furosemide is a commonly used diuretic to treat volume overload state in heart failure
but it is particularly prone to the problem of diuretic resistance because of its particular
pharmacokinetics.
Also, chronic diuretic use also induces hypertrophy in distal tubular cells, leading
again to enhanced sodium reuptake, contributing further to diuretic resistance.
Alternatives to furosemide, such as torsemide, have been shown to have a slight
advantage in selected studies because of somewhat more favourable pharmacokinetics.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Ans : Patients with cardiorenal syndrome are known to have systemic inflammation
There is an inflammation of monocytes and other inflammatory cells. This puts the
patient in an immune suppressive state, chances of infection are increased.
To reduce the chances of infection, as a prophylactic measure, ceftriaxone might have
been started.
GASTROENTEROLOGY CASES-
CASE 1
A 33 year old male with pain abdomen, vomiting, constipation, burning micturition and fever.
.https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html
5YEARS AGO : An episode of pain abdomen and vomitings,
Treated conservatively at a local hospital.
Stopped alcohol consumption.
↓
Symptom free for almost 3 YEARS
Patient started consuming alcohol, this lead to recurrent episodes of
pain abdomen and vomiting.
1 YEAR AGO : 5-6 episodes of pain abdomen and vomitings
Treated by a RMP.
↓
1 WEEK AGO : Binge of alcohol
↓
SINCE 1 WEEK : pain abdomen and vomitings.
↓
SINCE 4 DAYS : High grade fever with chills and rigors
Developed constipation
Burning MICTURITION associated with subrapubic pain , increased
frequency and urgency.
➤ Anatomical localisation : GASTROINTESTINAL SYSTEM.( stomach and pancreas
mainly as the symptoms suggest)
➤ Etiology : the patient is a chronic alcoholic, episodes of abdominal pain and vomiting
are following alcohol consumption .
THEREFORE it is heavy drinking that has led to the above condition in the
patient.
2. What is the efficacy of drugs used along with other non pharmacological treatment
modalities and how would you approach this patient as a treating physician?
Ans :Drugs used in this patient -
➣ ING. MEROPENEM ; TID for 7 days
Meropenem is a broad spectrum carbipenem antibiotic used to treat abdominal and
skin infections.
BASED ON A STUDY-In patients with moderate to severe intra-abdominal infections,
empirical monotherapy with meropenem achieved clinical response rates ranging from
91 to 100% in 7 randomised comparative trials. Meropenem also achieved clinical
response rates of over 80% in patients with severe intra-abdominal infections.
➣ING. METROGYL 500 mg IV TID for 5 days
Composition- METRONIDAZOLE.
Metronidazole belongs to Nitroimidazole group of antibiotics, is used to treat
gastrointestinal infections, skin and blood infections.
Based on the above study metronidazole when combined with another antimicrobial
agent is more effective in the treatment of complicated intra abdominal infections
( particularly those caused by ENTEROBACTERIACEAE MEMBERS as they are
resistant to carbipenem).
➣ING. AMIKACIN 500 mg IV BD for 5days
.AMIKACIN is an amino glycoside antibiotic used in the treatment of serious bacterial
infections.
All the above three antibiotics are given to control infection and prevent sepsis in the
patient.
➣ING. OCTREOTIDE 100 mg SC , BD
Octreotide is a long acting analogue of Somatostatin
.It inhibits exocrine secretion of the pancreas, also has anti inflammatory and
cytoprotective effects.
EFFICACY - Octeotride based on several studies did not provide any symptomatic relief
or better cure when compared to other drugs . However it played a significant role in
reducing SERUM AMYLASE AND LIPASE LEVELS.
➣ ING. PANTOP 40 mg IV , OD
Pantoprazole a proton pump inhibitor, is known to have pancreatic anti secretory effect.
Oxidative stress is common in acute pancreatitis- Pantoprazole has a inhibitory effect
on hydroxy radicals ( free radicals )- thereby reduces the progression of the disease and
helps in reducing oxidative stress.
PPZ treatment also reduces tissue infiltration of inflammatory cells and acinar cell
necrosis in severe AP.
➣ ING. TRAMADOL in 100 ml NS IV , OD
Tramadol is an opioid analgesic used to relieve severe pain in acute pancreatitis.
➣ING. THIAMINE 100 mg in 100 ml NS IV , TID.
Thaimine - Vitamin B1 supplement.
As the patient is on TPN there is a chance of B1 deficiency
Wernicke’s encephalopathy ( due to B1 deficiency) has been noted in several cases of
pancreatitis so to prevent this Thiamine is given as a prophylactic measure
➣ TPN ( Total Parenteral Nutrition )
(TPN) is a method of feeding that bypasses the gastrointestinal tract. Fluids are given
intravenously to provide nutrients the body needs. The method is used when a person
cannot or should not receive feedings or fluids by mouth.
Parenteral nutrition is used to prevent malnutrition in patients who are unable to obtain
adequate nutrients by oral or enteral routes.
MY APPROACH TO THIS PATIENT AS A TREATING PHYSICIAN:
-When the patients present with the complaints of pain abdomen and vomiting, along with
fever, burning micturition, certain investigations must be done.
- First, a general examination must be done, including inspection, percussion, palpation and
auscultation of the abdomen.
-Other investigations are CBP (Complete Blood Picture ), LFT( Liver Function tests ),
RFT( Renal Function Test ) , Urine analysis, Serum amylase, ABG( Arterial Blood Gas ),
Pleural tapping.
-Some imaging studies like, contrast enhanced CT and chest x-ray should be taken as well.
Now depending on the diagnosis based on the results, chemotherapy must be started. In
the case of pancreatitis in this patient, the following treatment can be given.
-- Antibiotic like MEROPENAM, METROGYL, AMIKACIN
- Fluid levels should be maintained with RL or NS
--Somatostatin analogue like SOMATOSTATIN, decreases the exocrine secretion in the
pancreas.
-- Proton pump inhibitor
--Vitamins such as Thiamine
--Anti-analgesic such as TRAMADOL.
CASE 2
A 25 year old man with epigastric pain.
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-25-year-old-male.html
1.What is causing the patient's dyspnea? How is it related to pancreatitis?
Ans :In case of severe pancreatitis, a lot of inflammatory chemicals that are secreted into
the blood stream. These chemicals create inflammation throughout the body, including
the lungs. As a result, a person may experience an inflammatory type of reaction in the
lungs called ARDS this results in dyspnoea in the patient.
2. Patient is a known alcoholic with increased consumption since 2 months (2 litres of
toddy everyday) this results in carbohydrate spike and can lead to diabetes in the patient.
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
CASE 3
A 45 year old female with fever, pain abdomen, decreased urine output and abdominal distension.
https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
1. What is the most probable diagnosis in this patient?
Ans : Based on the symptoms shown by the patient :
Differential Diagnosis-
• Ruptured Liver Abscess.
• Organized Intraperitoneal Hematoma
.• Organized collection secondary to Hollow viscous Perforation.
The most probably diagnosis is presence of abdominal hemorrhage. This will give reasoning to the abdominal distention, and the blood which is aspirated.
2. What was the cause of her death?
Ans : After discharge from the hospital, the patient went to Hyderabad and underwent an
emergency laparotomy surgery. The patient passed away the next day.
Cause of her death could be complications of laparotomy surgery such as
bleeding, infection, or damage to internal organs.
2. Why does he have intermittent episodes of drowsiness?
Ans : The intermittent episodes of drowsiness in this patient could be due to Hyponatremia.
* Due to Hyponatremia, serum sodium levels are low, low sodium serum levels affect
several biological pathways in the nervous system and can cause neurological
impairment.
* Due to low serum sodium levels there is is low extracellular osmolality, this results in
swelling of all cells in the body including brain cells.
This is be the reason for drowsiness in the patient.
3. Why did he complaint of fleshy mass like passage in his urine?
Ans :The patient in this case has a history of dysuria and urine is cloudy in appearance. On
investigation, there is a presence of pus cells in the urine. The patient has an indication
of hydronephrosis, which is a condition that typically occurs when the kidney swells due
to urine failing to properly drain from the kidney to the bladder.
Due to stasis of fluid, these patients become predisposed to development of urinary tract
infection (UTI), which can be the cause of fleshy type masses or gritty particles in the
urine.
Bladder injury
Infection
Bleeding
Electrolyte abnormalities
Painful or difficult urination
CASE 2
An eight year old with frequent urination.
https://drsaranyaroshni.blogspot.com/2021/05/an-eight-year-old-with-frequent.html
1.Why is the child excessively hyperactive without much of social etiquettes ?
Ans : According to the case history, the patient, in this case is an 8 year old boy, is excessively
hyperactive, impulsive, does not have proper social etiquettes as is expected of his age,
too active to pay any attention at school, talk so fast that even comprehending sentence
becomes quite difficult.
These issues are ongoing in the boy, and are prominent enough to be negatively
affecting his daily life. This prompts one to consider the possibility of the boy having
ADHD (attention deficit hyperactivity disorder).
People who have ADHD have combinations of these symptoms:
• Overlook or miss details, make careless mistakes in schoolwork, at work, or during
other activities.
• Have problems sustaining attention in tasks or play, including conversations, lectures,
or lengthy reading
• Seem to not listen when spoken to directly.
• Avoid or dislike tasks that require sustained mental effort, such as school homework.
Signs of hyperactivity and impulsivity may include:
• Fidgeting and squirming while seated
• Running or dashing around or climbing in situations where it is inappropriate, or, in
teens and adults, often feeling restless
• Talking nonstop
• Blurting out an answer before a question has been completed, finishing other people’s
sentences, or speaking without waiting for a turn in conversation
(Reference link- https://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder-adhd-the-basics/)
2. Why doesn't the child have the excessive urge of urination at night time ?
Ans : The child in this case has gotten a series of tests done in order to come to a conclusion
about his diagnosis.
a) Urine examination of the child is completely normal.
b) The child shows symptoms of ADHD this could lead to hyperexcitability, since its
only happening during the day time it could also be psychosomatic.
3. How would you want to manage the patient to relieve him of his symptoms?
Ans : The diagnosis of the child is pointing towards the possibility of a psychosomatic
overactive bladder, which can be triggered by various stressors or the possibility of the
child having undiagnosed ADHD. In either of these cases, change in the daily habits
and behavior, along with conservative therapy such as bladder exercises will provide
relief before doing medical or surgical intervention.
The most common treatment options include bladder retraining and pelvic floor
exercises.
. If these techniques do not work or seem to have no effect on the overactive
bladder, medications can be used to calm the overactive bladder like oxybutynin .
INFECTIOUS DISEASES -
CASE
A 40 year old female with dysphagia, fever and cough.
https://vyshnavikonakalla.blogspot.com/2021/05/a-40-year-old-lady-with-dysphagia-fever.html
Ans : The characteristic features of TEF in adults are- recurrent pneumonia, hemoptysis, and
coughing after eating.
In children, the features found in cases of congenital tracheoesophageal fistula- is
frothy, white bubbles in the mouth, coughing or choking when feeding, vomiting,
cyanosis especially when the baby is feeding, difficulty breathing.
The physical finding in the presence of TEF is abdominal distention which may occur
secondary to collection of air in the stomach.
2. What are the chances of this patient developing immune reconstitution inflammatory
syndrome? Can we prevent it?
positive. She is more susceptible to any infection and therefor prone to reinfection.
To prevent IRIS, the most effective method is to involve the initiation of ART before
immunosuppression is advanced.
IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-
cell count greater than 100 cells/uL.
INFECTIOUS DISEASE AND HEPATOLOGY CASES-
CASE 1
A 55 year old male with pain abdomen, decreased appetite and fever.
https://kavyasamudrala.
Toddy is a locally brewed beverage, when the conditions are unhygienic it gets
contaminated with bacteria, fungi, parasites.Of particular contamination with
ENTAMOEBA HISTOLYTICA is known to cause liver abscess.
Based on his occupation the patient belongs to low socio economic group - so chances
of malnutrition is more this further favours the survival of the parasite.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30
years - 1 bottle per day)
Ans : Alcohol causes AMOEBIC LIVER ABSCESS(ALA) through a multitude of
mechanisms:
- Alcohol induced hepatic dysfunction
- It lowers body resistance and suppresses immune mechanisms in the habitual consumers.
- Locally prepared alcohol ( toddy) when brewed in unhygienic conditions may be contaminated by pathogens ( bacteria, parasites- ENTAMOEBA HISTOLYTICA.)
- Toddy has very less alcoholic content (< 5%) - this favours the survival of Entamoeba and promotes the conversion of latent forms to virulent forms resulting in more symptomatic cases.
- alcohol-induced hepatic dysfunction and possible suppression of amoebistatic immune mechanisms by substances in the beverages could also be attributed in the mechanism.
The involvement of right lobe to left lobe is in the ratio of 2: 1
Liver abscess is more common in the right lobe than left lobe because
- The right hepatic lobe receives blood from both the superior mesenteric and portal veins, whereas the left hepatic lobe receives inferior mesenteric and splenic drainage
- It also contains a denser network of biliary canaliculi and overall more hepatic mass.
- Presence of a left lobe abscess of more than 10cm in diameter.
- Pain and impending rupture.
- Abscess that does not respond to medical treatment within 3-5 days.
Toddy ( a local alcoholic beverage) when collected in unhygienic environment, might
get contaminated with pathogens such as bacteria, parasites ( Entamoeba histolytica).
These pathogens through portal circulation reach the liver and might result in
ABSCESS formation in the patient.
2. How do you approach this patient ?
Ans : . When patient presents with chief complaints of abdominal pain , fever -
- Detailed history regarding each of the symptom should be taken.
- General examination to know the overall health status should be carried out.
- Following general examination, systemic examination ( CVS, RESPIRATORY, PER ABDOMEN, CNS) should be done.
Patient’s symptoms point out to the involvement of GASTROINTESTINAL SYSTEM,
therefore special emphasis should be on per abdominal examination.
4. Through history and examination , we arrive at provisional diagnosis.
5. To confirm the diagnosis, investigations, imaging tests should be taken.
6. For this patient based oh his sympatology, the following investigations should be done.
CBP, LIVER FUNCTION TESTS, RENAL FUNCTION TESTS, URINE ANALYSIS.
7. Imaging tests- CXR, USG abdomen.
Based on the results of these the diagnosis can be confirmed, treatment can be initiated.
This patient is diagnosed with LIVER ABSCESS ( by the above approach) , the
following treatment can be given.
. In practice an empirical treatment is given to treat both amoebic and pyogenic
liver abscess
*This includes use of Broad spectrum antibiotics( for pyogenic liver abscess) ,
*Metronidazole ( for amoebic liver abscess)
* Analgesics and anti inflammatory drugs -to relieve pain and fever.
* Multivitamin supplements
*Saline infusion- to maintain fluid levels.
All the above medicines should be given for 7- 10 days.
Following this review the patient and see if there is any improvement.
-USG abdomen should be done se if the abscess is resolving.
-Investigations ( CBP, LFT , RFT ) should be done to check for the improvement.
-If the abscess did not resolve ULTRASOUND GUIDED ASPIRATION SHOULD
BE DONE.
3. Why do we treat here ; both amoebic and pyogenic liver abcess?
Ans :The presentation for both amoebic , pyogenic liver abscess is the same i.e, pain
abdomen, fever, constitutional symptoms like nausea and vomitimg, loss of appetite,
in some cases there may be pulmonary symptoms.
INVESTIGATIONS-
There is leucocytosis, elevated alkaline phosphatase ,ALT, AST
USG-a hypo echoic mass for both type of abscess.
-Amoebic and pyogenic liver abscess can be differentiated only by culture and
sensitivity of the aspirate obtained by USG GUIDED ASPIRATION OF THE
ABSCESS.
-USG GUIDED ASPIRATION has the following risk factors associated with it:
1) if abscess is thin walled there is a risk of rupture.
2)if abscess is on the posterior aspect of the liver, it will not be accessible.
3)there is also a risk of bleeding.
. Blood culture taken prior to the administration of antibiotics is helpful for identifying
the causative organism but as this patient had already taken antimicrobials before he
came to the hospital, there is severe abdominal pain treatment is started immediately
without a blood culture report.
Considering that it is difficult to distinguish amoebic liver abscess from pyogenic
liver abscess, we treat both forms of Liver abscess empirically using-
- Broad spectrum antibiotics- a combination of penicillin , cephalosporin, ahminoglycosides
- Metronidazole- has both antibacterial and antiprotozoal activity.
Liver abscess: diagnostic and management issues found in ...https://academic.oup.com › bmb › article
This article highlights the difficulties in distinguish the two forms of liver abscess.
4. Is there a way to confirm the definitive diagnosis in this patient?
Ans : Liver abscess can be confirmed by USG ABDOMEN - it presents as single / multiple,
round / oval , hypoechoic - hyper echoic mass more commonly is the right lobe of the
liver.
However USG cannot differentiate an amoebic liver abscess from pyogenic liver
abscess.
*Blood culture
*USG guided aspiration of the abscess should be done.
This aspirate should be subjected to antigen testing for - Entamoeba histolytic
Subjected to microbiological culture and sensitivity - to identify pyogenic organisms.
INFECTIOUS DISEASE CASE -
(Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology)
A 50 year old male with altered sensorium.
http://manikaraovinay.blogspot.com/2021/05/50male-came-in-altered-sensorium.html
1. inj. Liposomal amphotericin B according to creatinine clearance
2. 200mg Iitraconazole was given as it was the only available drug which was adjusted
to his creatinine clearance.
3. Deoxycholate was the required drug which was unavailable
https://pubmed.ncbi.nlm.nih.gov/23729001/
This article talks about the efficacy and toxicity of different formulations of amphotericinB
along with the above mentioned treatment for the patient.
Management of diabetic ketoacidosis –
(b) Electrolyte replacement-The absence of insulin can lower the level of several electrolyte
in blood. Patient will receive electrolytes through a vein to help keep the heart, muscles
and nerve cells functioning normally.
(c) Insulin therapy- Insulin reverses the processes that cause diabetic ketoacidosis. In
addition to fluids and electrolytes, patient will receive insulin therapy.
3. What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
for the treatment of severly ill and critical Covid 19 patients. Steroids reduce
inflammation in the lungs, stop some of the damage that can happens when the body's
immune system goes into overdrive to fight off coronavirus. But at they also reduce
immunity and push up blood sugar levels in both diabetics and non-diabetic Covid-19
patients.
With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in
these patients is increasing.
INFECTIOUS DISEASE- COVID 19-
Link to the COVID master chart.
https://drive.google.com/file/d/120TmHdHgV_yu77K6JPjuE__H2F7vJwQ5/view?usp=sharing
















I want to share with you all on how Dr Itua saves my life with his powerful Herbal medicines, I was diagnosed of Oral/Ovarian Cancer which i suffered from for 5 years with no positive treatment until when My son came to me in the hospital when i was laying down on my dying bed waiting for god to call out my name to join him in heaven.
ReplyDeleteMy son was so excited that very day he came across Dr Itua on Blogspot, we decided to give him a try although we Americans are so scared to trust Africans but i really have no choice that time to choose life in between so we gave a try to Dr Itua Herbal medicines, god willing he was a good man with a god gift. Dr Itua sent us herbal medicine. It was three bottles. I took it for three weeks as an instructor and these herbal medicines heal me, cure my Oral/Ovarian Cancer completely. I have been living for 9 months now with a healthy life with no more symptoms.
I'm sponsoring Dr Itua in LA Advert on Cancer patent seminar which my son will be participating too and other patent Dr Itua has cured from all kind of human disease, also if you are sick from disease like,Epilepsy,Breast Cancer,Prostate Cancer,Throat cancer,Thyroid Cancer,Uterine cancer,Fibroid,Angiopathy, Ataxia,Arthritis,Brain cancer,Hiv,. Vaginal cancer,Herpes,Colon-Rectal Cancer,Chronic Disease.Amyotrophic Lateral Sclerosis,Brain Tumor,Fibromyalgia,Fluoroquinolone Toxicity,Multiple myeloma,Tach Diseases,Leukemia,Liver cancer,
Esophageal cancer,Gallbladder cancer,,Bladder cancer,Gestational trophoblastic disease,Head and neck cancer,Hodgkin lymphoma
Intestinal cancer,Kidney cancer,Hpv,Lung cancer,Adrenal cancer.Bile duct cancer,Bone cancer,Melanoma,Mesothelioma,Neuroendocrine tumors
Non-Hodgkin lymphoma,Cervical Cancer,Oral cancer,Hepatitis,Skin cancer,Soft tissue sarcoma,Spinal cancer,Pancreatic Cancer, Stomach cancer
Testicular cancer,
Syndrome Fibrodysplasia Ossificans ProgresS sclerosis,Alzheimer's disease,Chronic Diarrhea,Copd,Parkinson,Als,Adrenocortical carcinoma Infectious mononucleosis,Vulvar cancer,Ovarian cancer,,Sinus cancer, Here Is The Wonderful Healer Contact. Name_ Doctor Itua, Email Contact: drituaherbalcenter@gmail.com, Phone/WhatsApp: +2348149277967